Dental Unit Waterline Safety:
A Critical Component of Patient Care
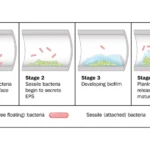
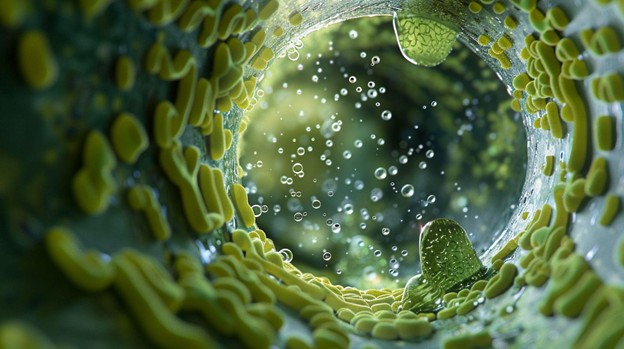
Why Do Dental Unit Waterlines Have Biofilm?
January 9, 2024
Biofilm: The Invisible Threat and Hidden Opportunities
September 5, 2024Dental Unit Waterline Safety:
A Critical Component of Patient Care
In a recent video interview with Kevin Henry, Editor in Chief of DrBicuspid.com, infection control expert Leslie Canham shed light on the importance of dental unit waterline safety and testing. As dental professionals, ensuring the quality of our dental unit waterlines is not just a regulatory requirement—it's a crucial aspect of patient care that can have far-reaching consequences if neglected.
The Importance of Dental Water Testing
Leslie emphasizes that testing treated dental unit water is essential to verify its safety. The goal is to maintain water quality at or below 500 colony-forming units (CFUs) of heterotrophic bacteria per milliliter, which is the EPA standard for safe drinking water. Without waterline testing, dental practices cannot be certain that their water treatment methods are effective.
What if I Fail a Test?
The best approach to treating dental unit water lines is to shock and test each chair on a monthly basis. If the tests are still failing after multiple shocks, consider treating your lines with Liquid Ultra.
Real-World Consequences of Waterline Contamination
The interview touched on several alarming incidents that underscore the importance of proper waterline maintenance. In Jonesboro, Georgia, a pediatric dental clinic experienced an outbreak where children became ill after undergoing pulpotomies. The cause was traced back to dental unit water contaminated with non-tuberculosis mycobacterium. Similarly, in Southern California, 73 children fell ill at the Children's Dental Group due to exposure to contaminated dental unit water. These cases serve as stark reminders that waterline contamination is not a theoretical risk but a real threat to patient safety.
While state dental boards may not always require testing and treatment of dental unit water, Leslie points out that following CDC guidelines and manufacturers' directions is crucial. In legal situations, juries will consider whether a dentist adhered to best practices in infection control during dental procedures.
Training New Team Members
With the influx of new dental team members, proper training in infection control is more important than ever. Leslie recommends utilizing resources from OSAP (Organization for Safety, Asepsis and Prevention, which was recently renamed to ADS: Association for Dental Safety), carefully reading and following manufacturer's instructions, and avoiding the pitfall of training new staff based on "the way we've always done it" rather than best practices.
Leslie strongly advocates for designating an Infection Control Coordinator in dental practices. This role is crucial for overseeing infection control protocols, staying updated on best practices, and communicating effectively with the team about infection control issues. Dental professionals should be prepared to have "courageous conversations" about infection control, bringing gaps in compliance to the attention of supervisors and practice owners.
Advancements in Dental Unit Waterline Treatment
The interview touched on the advantages of silver ion technology in waterline treatment, such as longer intervals between shock treatments, no taste issues for patients (unlike iodine-based treatments), and greater convenience for staff maintaining the waterlines.
As we move forward, Leslie hopes to see dental practices taking infection control more seriously by empowering team members with knowledge and tools, providing time and resources for proper infection control training, and creating an environment where staff feel comfortable raising concerns about infection control practices.
Conclusion
Dental waterline safety is not just about compliance—it's about protecting our patients and maintaining the integrity of our profession. By staying informed, following best practices, and fostering a culture of open communication about infection control, we can ensure that our dental practices remain safe environments for all who walk through our doors.
Remember, when it comes to infection control information, always rely on trusted sources like ADS (formerly OSAP) and manufacturer instructions rather than social media opinions. Your patients' safety depends on it.